
There is an ever-growing pathology that increasingly attracts the attention of the medical-scientific sector for the risks involved, but mainly due to the lack of an optimal remedy without side effects: hyperuricemia.
The data in this regard are precise: 10% of the adult population has a high uricemia level at least once in their lives (Passamont, M.). Furthermore, data dating back to 2009 show an incidence of 89.9 cases per 1000 assisted a particularly significant figure compared to 2005, which recorded a value of 67.3 cases per 1000 assisted. This is evidence of the rapid and continuous growth of the disease, underscoring the urgency of developing products that support people with it.
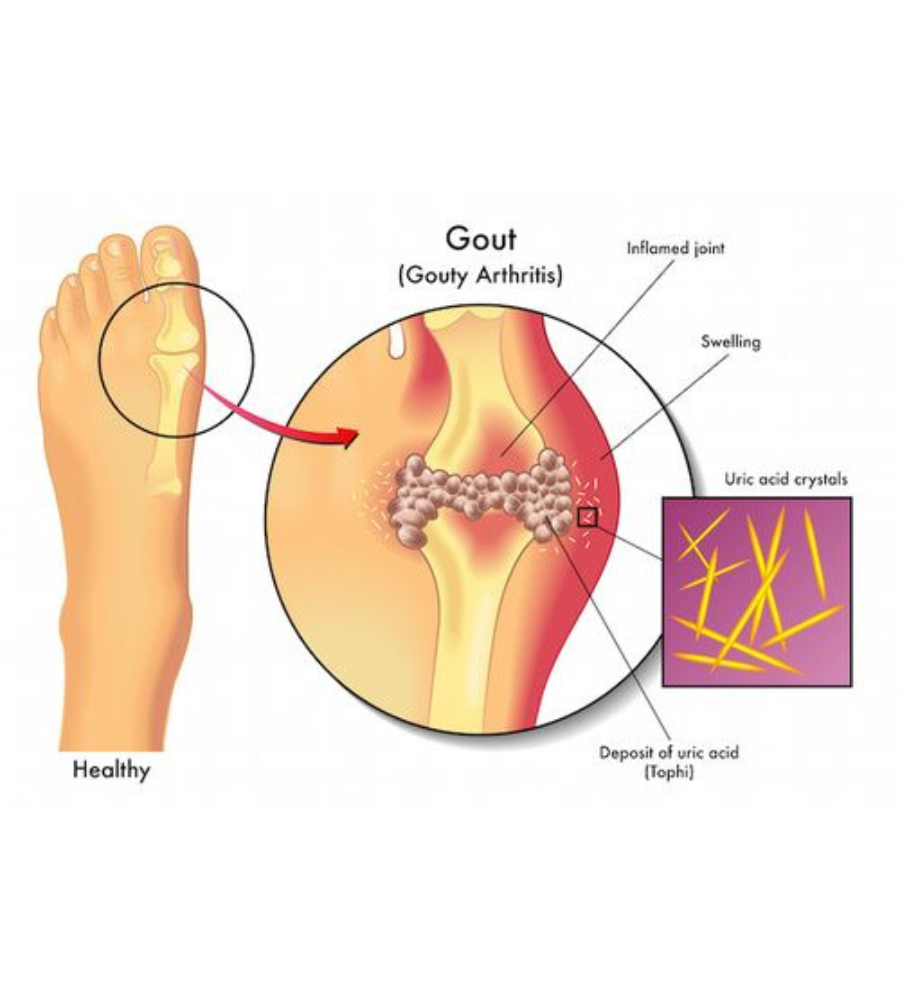
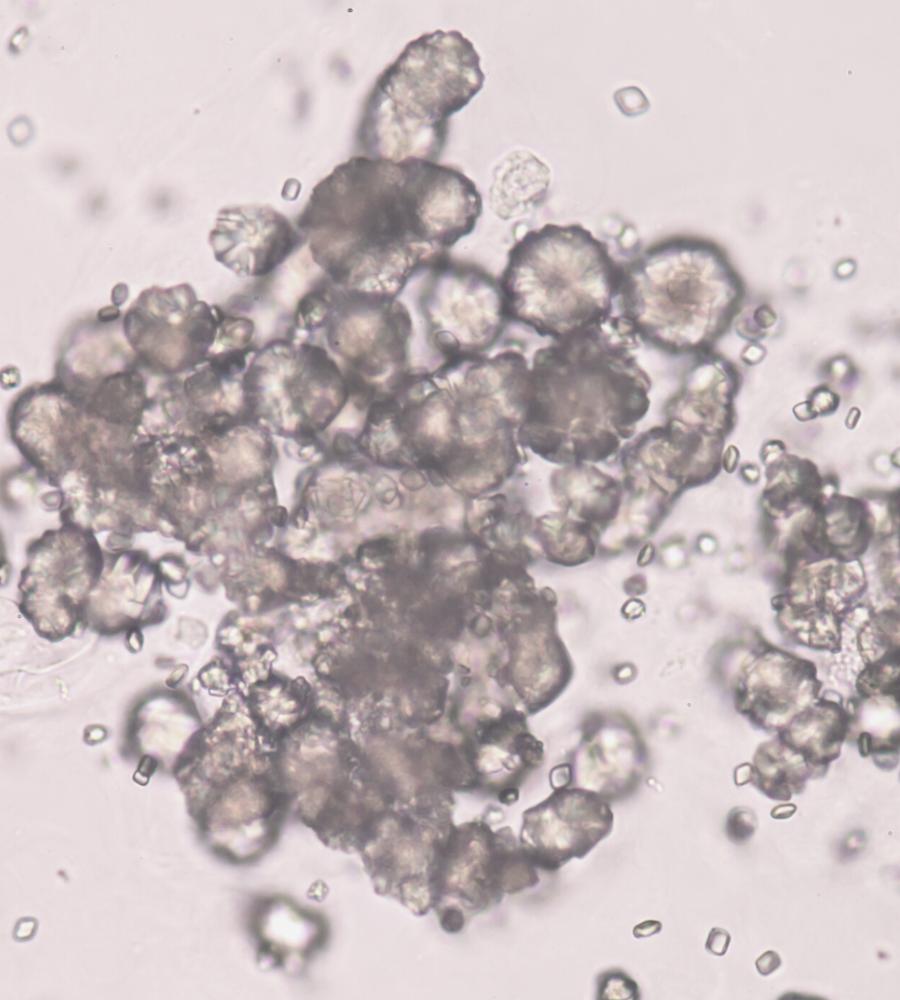
Hyperuricemia is a condition that occurs when the levels of uric acid present in the blood exceed the value of 6.8 mg/dL. Uric acid is a waste substance of cell metabolism, which is produced by the degradation of purines. When this substance accumulates, is released to excess, or is not eliminated sufficiently (through urine), its blood level increases.
For most hypouricemic subjects, it has been observed that the main defect is represented by a lower elimination of uric acid at the glomerular level. It has been proven that subjects with hyperuricemia and urate deposition have an excretion of uric acid reduced on average by 41% compared to the normal population.
The causes of hyperuricemia can be numerous and, therefore, difficult to identify with certainty. Among the risk factors, there are undoubtedly incorrect lifestyles, such as a diet rich in animal foods and usually rich in purines, obesity, excessive consumption of sugary drinks and alcohol, cancer and osteoarticular diseases, and kidney diseases like kidney failure, stones, and polycystic kidneys. In addition, chemotherapy treatments and prolonged use of diuretics may contribute to the development of the condition.
The consequences of hyperuricemia are numerous and diverse; therefore the medical community is increasingly interested in it. For example, a high uric acid level in the blood can be a risk factor for developing brain, kidney, and especially cardiovascular diseases. This appears to be of considerable importance if we consider that cardiovascular diseases represent the first cause of death in Western civilizations. Treating hyperuricemia is, therefore, also part of a broader primary prevention activity for cardiocerebrovascular risk.
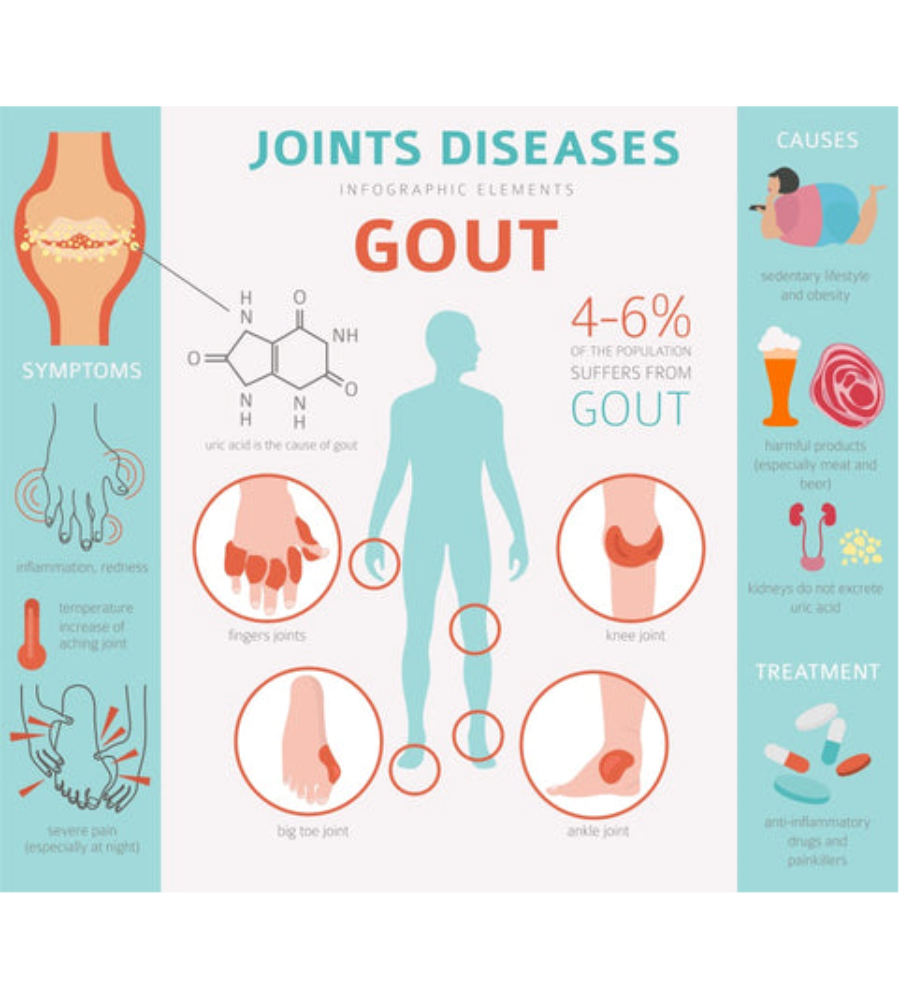
Hyperuricemia is also considered the leading cause of gouty arthritis.
Gout is considered one of the most painful forms of Rheumatism. It is an inflammation-related, precisely, to an accumulation of uric acid. This disease mainly affects men (80%), and in males over 40 years of age, gout is the most frequent inflammatory disease of the joints, while women are immune until menopause, as female hormones protect them.
Pathology develops slowly and asymptomatically until sudden acute manifestation. These events occur without warning, often at night, and mainly affect the big toe joint and surrounding skin, which become swollen, reddened, and extremely sensitive to touch and pressure.
The most frequent triggers of an acute gout crisis are linked to nutrition: large meals rich in meat, excessive consumption of alcohol, extreme diets, or slimming treatments. In addition, in hospitalized patients, gout attacks may occur after taking diuretic medications that may be necessary to reduce blood pressure or relieve circulation. While increasing the amount of urine, these drugs do not allow the expulsion of a more significant amount of uric acid.
In the case of hyperuricemia, the patient may experience pain caused by gout in waves and at shorter and shorter intervals. Without treatment, this situation can degenerate into chronic gout, damage the different joints simultaneously and lead to the formation of unsightly gouty nodules or harmless deposits of urate crystals in the coldest parts of the body, such as the auricle, elbows, feet, and fingers. In addition, chronic gout can result in uric acid deposits in the kidneys. The kidney stones that form can inflame the renal pelvis and cause colic. In addition, chronic gout can degenerate into so-called secondary arthrosis.
A fundamental part of the treatment path of hyperuricemia is undoubtedly a change in lifestyle and, specifically, a correction of those habitual ones that we have already defined as risk factors. The achievement of an ideal body mass index, the cessation of cigarette smoking, the increase in physical exercise, and the maintenance of good hydration associated with a reduction in the use of alcohol and foods rich in purines are, therefore, crucial elements for achieving uricemia values below 6.5 mg/dl.
However, these measures may not be effective unless supported by a pharmacological or nutraceutical product. Despite the increasing prevalence of the disease, however, the range of drugs currently available is old-fashioned. Also, it corresponds to a lack of willingness on the part of patients to take the medications because of the side effects often encountered. The current treatment for hyperuricemia, which generally includes allopurinol or uricosuric, has important drawbacks, such as itching and rash, which occur in 3 to 10% of cases. Less frequently, fever, leucocytosis, hepatitis, and eosinophilia.
Therefore, there is a need for a new, effective, and safe product. This need was the engine that pushed Biofarma Group to develop a nutraceutical able to support all people suffering from this condition, minimizing side effects.
Biofarma Group conducted a clinical study published in the “Journal of Food and Nutrition Research” to develop a supplement to lower uric acid in the blood in patients with a borderline situation of hyperuricemia.
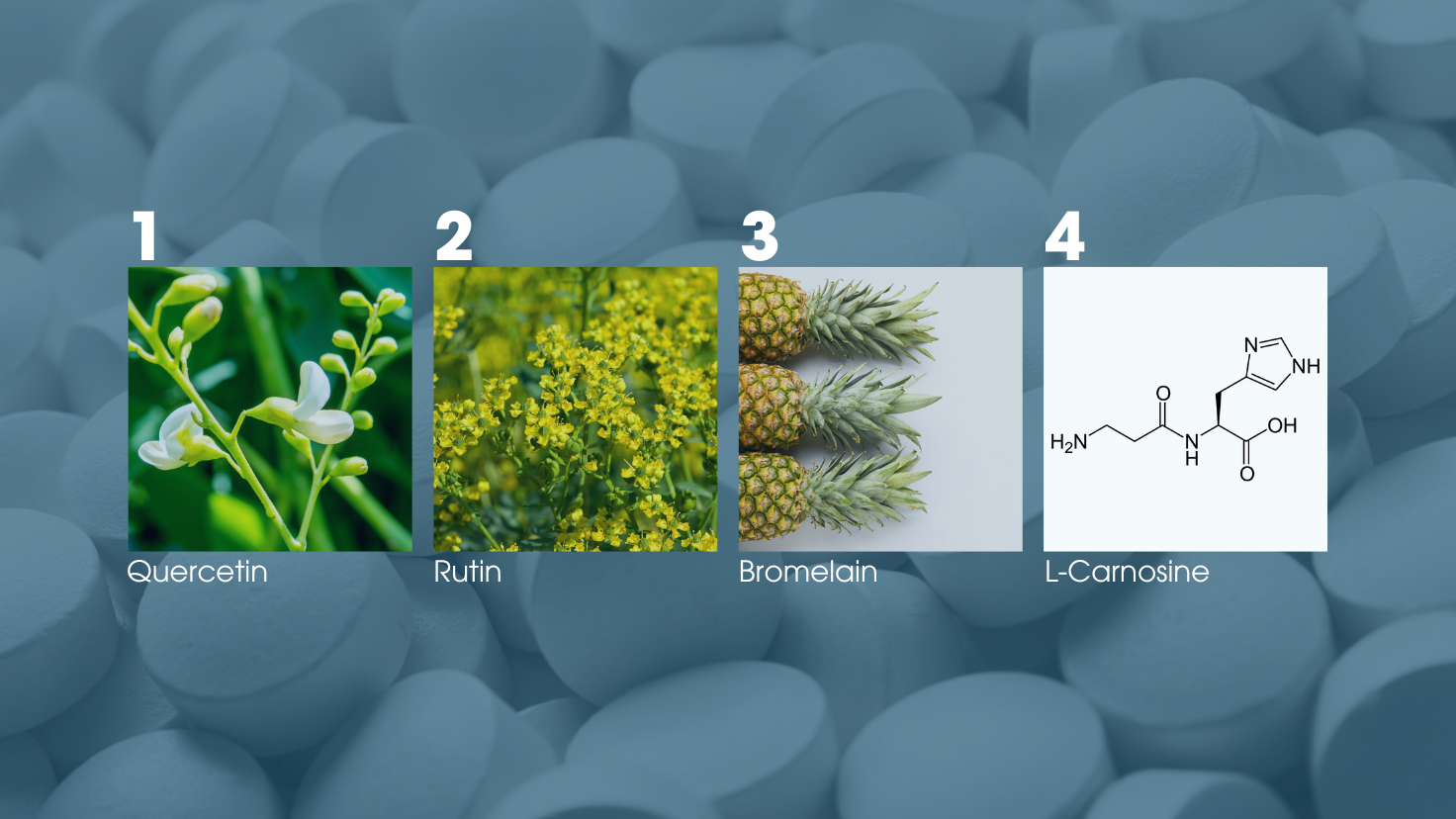
Specifically, a trial was structured whose purpose was to observe the effects produced by a nutraceutical containing quercetin, rutin, bromelain, and L-carnosine in subjects with uric acid levels between 6 and 7 mg/dl.
A total of 116 patients were selected for the study who were asked to take a placebo or nutraceutical for three months, once daily at breakfast time. At the end of the study, an effective reduction in uricemia was observed in the nutraceutical–treated group relative to the baseline condition and the placebo group. Specifically: at baseline, 55.9% of patients had uric acid levels between 6.5 and 7.0 mg/dl versus 0% after three months of treatment; At the end of the trial, 67.3% had uric acid levels between 6.0 and 6.4 mg/dL versus 44.1% at baseline; In 32.7% I had uric acid levels between 5.5 and 5.9 mg/dL, compared with 0% at baseline. As for the placebo group, no significant changes were observed.
The study then confirmed the efficacy of the nutraceutical Uricemin® in lowering the values of uric acid in the blood. This effectiveness is given by the four mechanisms of action of its components: quercetin which inhibits the activity of the enzyme that favors the final reaction of the synthesis of uric acid; rutin increases the renal secretion of urate; bromelain, which has analgesic and anti-inflammatory properties; finally, L-carnosine can modulate the reabsorption of uric acid, thus reducing the levels in the blood.
The result of the research and development laboratory of Biofarma Group is, therefore, an innovative tablet able to counteract hyperuricemia in patients with borderline uric acid levels, especially without side effects.
Edited by:
Arianna Vanelli: R&D Manager
Stefania Murzilli: Scientific Specialist
Derosa G., D’angelo A., Maffioli P., “Evaluation of the Effects of a Supplement Composed by Quercetin, Rutin, Bromelain and L-Carnosine in Patients with Borderline Uricemi”, Journal of Food and Nutrition Research, 2020
Frei P., “Gout and pseudogout,” Swiss League which fights Rheumatism
Passamonti M., “Asymptomatic hyperuricemia. The new addresses: what to know to act well in General Medicine”, MeDia 2015